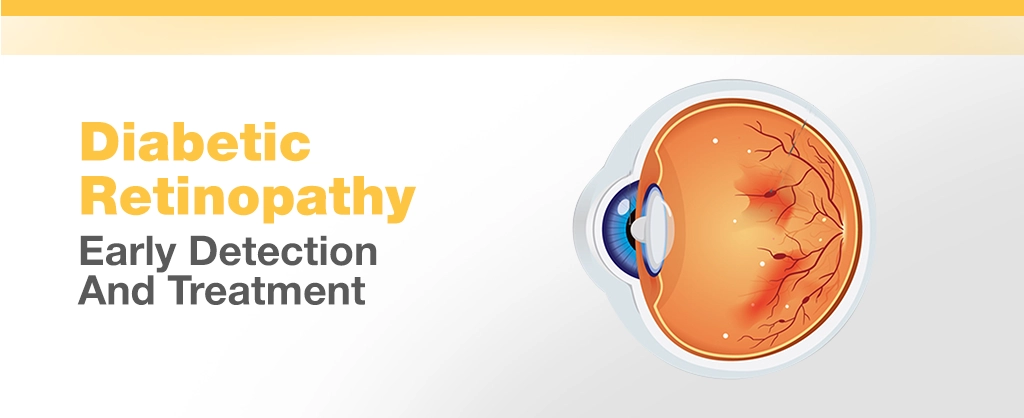
Diabetes is more than a disease that controls blood sugar; it has widespread effects throughout the body. One of the most dangerous complications is diabetic retinopathy, a chronic eye disease that can result in vision loss and even blindness. It tends to develop unobtrusively and gradually, so early detection is important to save one’s vision.
This blog will take you through what diabetic retinopathy is, its symptoms, stages, and most importantly, how it can be detected early and treated successfully. We will also mention prevention tips and what you need to know if you are at risk.
Read Also: How to Improve Eyesight Naturally? Eye Care Tips
What is Diabetic Retinopathy?
Diabetic retinopathy is a diabetes complication affecting the eyes. It results from high blood sugar levels over time damaging blood vessels in the retina—the light-sensitive tissue at the back of the eye. These weakened vessels will leak blood or fluid, become inflamed, or become completely blocked, causing vision reduction or distortion. Eventually, new, unstable blood vessels may develop, further adding to vision loss.
It affects Type 1 and Type 2 diabetics alike and can develop without any warning signs in its initial stages. Diabetic retinopathy is ranked among the top causes of preventable blindness for working-age adults globally, as per the International Diabetes Federation.
Read Also: 10 Signs You Need An Eye Checkup (Don’t Ignore These!)
What are the Early Symptoms of Diabetic Retinopathy?
Identifying the initial signs of diabetic eye disease is difficult since most patients don’t notice changes in their vision at the early stage. Nonetheless, as the condition gets worse, some manifestations will start to develop, such as:
- Blurry or changing vision
- Trouble seeing at night
- Dark spots or blanks in your vision
- Floaters or dark spots
- Colors looking pale or washed out
Since these signs and symptoms are usually slow in developing, they go unnoticed. Eye check-ups are thus important for individuals with diabetes.
Read Also: Why Regular Eye Checkups Are Essential at Every Age
Stages of Diabetic Retinopathy
Diabetic retinopathy normally goes through four stages:
- Mild Non-Proliferative Retinopathy
This is the initial stage and is marked by microaneurysms, small balloon-shaped distensions in the retina’s blood vessels. There could be very little leakage of fluid, but vision remains normal.
- Moderate Non-Proliferative Retinopathy
At this point, blood vessels that supply the retina start swelling and becoming distorted. Some lose their function in carrying blood. Retinal swelling (edema) will begin to interfere with vision.
- Advanced Non-Proliferative Retinopathy
Additional blood vessels get blocked, starving the retina of vital nutrients. This shortage of oxygen triggers the retina to produce new blood vessels.
- Proliferative Diabetic Retinopathy (PDR)
It is the most developed phase. New, thin blood vessels form along the retina and into the vitreous (the gel in the middle of the eye). These vessels can bleed, leading to extensive loss of vision or blindness. Scar tissue can also form, which causes retinal detachment.
Read Also: Understanding Blurred Vision: Common Causes & Warning Signs
Diabetic Macular Edema (DME)
One of the frequent side complications of diabetic retinopathy is diabetic macular edema. The macula is the retina’s central portion that provides for sharp, central vision. Fluid seeps into the macula during DME, leading to swelling that distorts vision. DME may develop at any point during diabetic retinopathy but is more likely in advanced stages.
Read Also: How Aging Affects Your Vision & What You Can Do About It
How is Diabetic Retinopathy Diagnosed?
Early detection of diabetic retinopathy is key to preventing vision loss. Diagnosis typically involves a comprehensive eye exam, including:
- Dilated Eye Exam: Drops are placed in your eyes to widen the pupils, allowing the doctor to examine the retina and optic nerve.
- Fluorescein Angiography: A dye is injected into a vein in your arm, and a special camera takes images of the retina to detect leaking blood vessels.
- Optical Coherence Tomography (OCT): This is an imaging study that produces detailed, high-quality cross-sectional photographs of the retina to look for swelling, fluid leakage, or other abnormalities.
Individuals with diabetes should have a dilated retinal examination at least yearly, even if they do not have any visual symptoms.
Read Also: What Is Night Blindness? Symptoms, Causes And Treatment
Treatment of Diabetic Retinopathy
Treatment of diabetic retinopathy has improved over the past few years. The treatment varies according to the stage of the disease and with or without diabetic macular edema.
- Monitoring for Early Stages
In some mild or moderate cases, medication may not immediately be needed. Rather, effective management of diabetes, maintenance of blood sugar, cholesterol, and blood pressure within goals, can prevent progression or even halt it. Frequent eye exams are crucial to track any progression.
- Laser Photocoagulation
The most frequent treatment, laser photocoagulation, closes leaking blood vessels and reduces the size of abnormal ones. This treatment is good at slowing vision loss but most often doesn’t regain already lost vision.
- Anti-VEGF Injections
These medications, administered directly into the eye, inhibit a protein called vascular endothelial growth factor (VEGF), which is responsible for abnormal blood vessel growth. Anti-VEGF medications such as Avastin, Eylea, or Lucentis are frequently employed to treat diabetic macular edema and proliferative retinopathy.
- Corticosteroids
Steroid injections or implants can occasionally be employed to decrease inflammation and swelling of the macula. They are likely to increase the danger of cataracts or glaucoma, though.
- Vitrectomy
For more advanced diabetic retinopathy, eye surgery with a procedure called vitrectomy may be required. This is where blood and scar tissue are removed from the vitreous gel, restoring sight and stopping further damage.
Read Also: Daily Habits To Maintain Healthy Eyes And Good Eyesight
Laser Treatment for Diabetic Retinopathy
Diabetic retinopathy laser therapy is still a standard treatment for most patients, particularly those with proliferative phases or DME. It’s usually performed as an outpatient procedure with little pain. Focal laser treatment focuses on individual leaking vessels, while pan-retinal photocoagulation helps to treat the peripheral retina to reduce abnormal blood vessels.
Living with Diabetic Eye Disease
Having diabetic retinopathy is not a verdict of blindness. With new treatments and lifestyle modifications, most patients are able to lead normal, productive lives. Controlling your overall diabetes is the best way to safeguard your eyes.
- Keep HbA1c levels under 7%
- Have healthy blood pressure (<140/90 mmHg)
- Keep cholesterol levels in control
- Quit smoking
- Exercise on a regular basis
- Eat a healthy, balanced diet
How to Prevent Diabetic Retinopathy?
Preventing diabetic retinopathy includes long-term diabetes control and periodic eye examinations. Here’s what you can do:
- Annual Dilated Eye Exams: Even if your eyes feel fine, schedule them annually.
- Monitor Blood Sugar Levels: Monitor them using a glucometer or continuous glucose monitor.
- Control Hypertension and Lipids: Work with your doctor to maintain them at a healthy level.
- Healthy Lifestyle Choices: Follow a healthy diet, exercise regularly, and don’t smoke.
- Learn About It: Be informed about the warning signs and phases of diabetic eye disease.
What is the Importance of Regular Screening?
Regular eye checks can be the difference between early intervention and irreversible harm. Even when you believe your eyes are good, diabetic retinopathy can be developing silently. By the time symptoms have developed, extensive retinal damage has probably already occurred.
Role of Technology in Managing Diabetic Eye Disease
Improvements in diagnostic technology such as OCT and digital fundus cameras have made early diagnosis a possibility. Telemedicine is also used to perform retinal screening remotely in remote or underserved areas, making early diagnosis possible to larger areas.
Artificial intelligence is being increasingly used to interpret retina scans and alert on abnormalities to help ophthalmologists make faster and more accurate diagnoses.
Conclusion
Diabetic retinopathy is a preventable but serious complication of diabetes. If discovered early and with proper eye care and medical therapy, the risk of loss of clear vision can be significantly reduced. If you have diabetes, don’t wait for symptoms to appear, receive regular eye examinations and take preventive steps against vision loss.
Click Here to Book Your Appointment Now.
Disclaimer
This content is for educational purposes only and does not replace professional medical advice. Please consult a qualified ophthalmologist to determine whether LASIK eye surgery is suitable for you.